IUI:
Intrauterine insemination (IUI) is a fertility treatment that involves placing prepared sperm directly into a woman’s uterus. It can be performed in both natural and stimulated menstrual cycles. The procedure is timed to coincide with ovulation, and the success rates can vary depending on individual circumstances
The success rates of IUI can vary depending on various factors, including the underlying cause of infertility, age, and the quality and quantity of sperm. IUI is often recommended for couples with mild male factor infertility, unexplained infertility, or certain cervical or ovulatory issues.
It is important to note that IUI is not recommended for severe male factor infertility, blocked fallopian tubes, or significant female fertility issues. In such cases, other fertility treatments such as in vitro fertilization (IVF) may be more appropriate. It is important to consult with a fertility specialist to determine the most suitable treatment approach based on the specific fertility factors involved.
In Vitro Fertilization (IVF):
In vitro fertilization (IVF) is a widely used and advanced fertility treatment that involves combining eggs and sperm outside the body in a laboratory setting. It is often recommended for couples who have difficulty conceiving naturally or for individuals who may require assistance in achieving pregnancy. Here is an overview of the IVF process:
- Ovarian Stimulation:
The woman undergoing IVF treatment is given fertility hormones, usually in the form of daily injections, to stimulate the ovaries to produce multiple eggs. The purpose of ovarian stimulation is to increase the number of mature eggs available for fertilization. - Egg Monitoring and Retrieval:
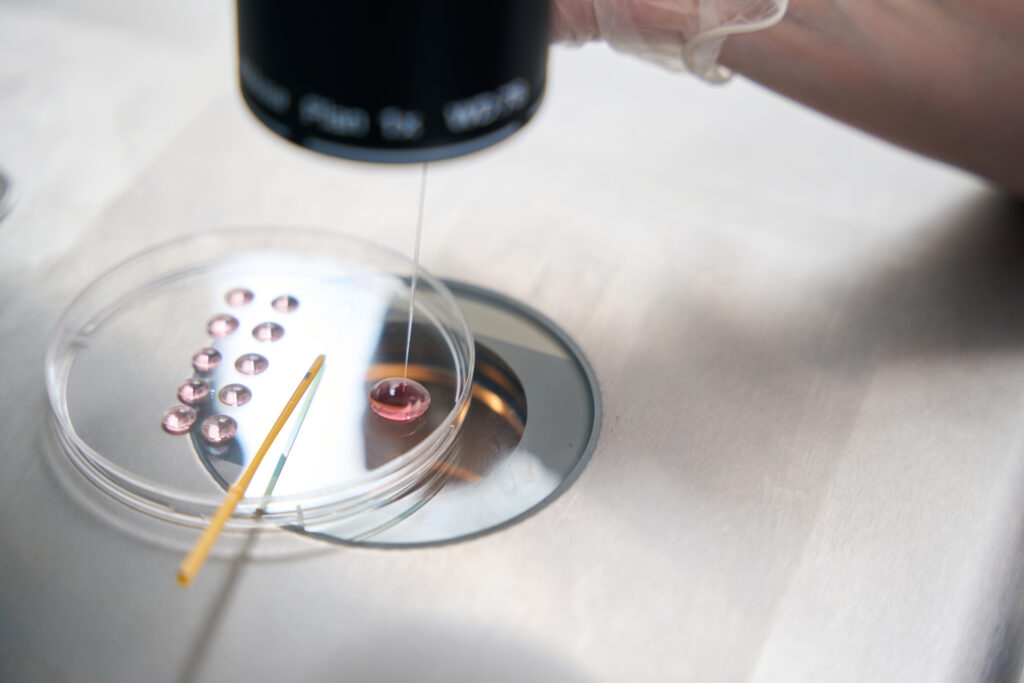
During the ovarian stimulation phase, the growth and development of the eggs are closely monitored using vaginal ultrasound scans and, in some cases, blood tests. Once the eggs have reached a certain size and maturity, an egg retrieval procedure is performed. This procedure is typically carried out under light sedation to minimize discomfort. A needle is guided through the vaginal wall to collect the eggs from the ovarian follicles. - Fertilization and Embryo Development:
After the eggs are retrieved, they are mixed with sperm in a laboratory dish to facilitate fertilization. In some cases, a technique called intracytoplasmic sperm injection (ICSI) may be used, where a single sperm is injected directly into an egg to enhance fertilization. Following fertilization, the embryos are cultured in a specialized incubator for a period of two to six days. During this time, the embryos are monitored for their development and quality. - Embryo Transfer:
Once the embryos have developed, the best-quality embryo(s) are selected for transfer to the woman’s uterus. The embryo transfer is a procedure where a thin catheter is guided through the cervix and into the uterus, and the selected embryo(s) is placed in the uterine cavity. The number of embryos transferred can vary depending on factors such as the woman’s age, embryo quality, and specific circumstances. The transfer is usually performed without anesthesia.
- Cryopreservation (Freezing):
Any additional good-quality embryos that are not transferred can be cryopreserved (frozen) for future use. This allows for subsequent embryo transfers without the need for additional ovarian stimulation and egg retrieval procedures.
Considerations:
Multiple Embryo Transfer: Transferring more than one embryo can increase the chances of pregnancy, but it also carries a higher risk of multiple pregnancies, such as twins or triplets. The decision on the number of embryos to transfer is often based on factors such as the woman’s age, embryo quality, and the desire to achieve a successful pregnancy while minimizing the risk of multiple gestations.
Health Considerations: Multiple pregnancies, especially higher-order multiples, can increase the risk of complications for both the mother and the babies, including premature birth and associated health issues. The decision-making process regarding the number of embryos to transfer should involve discussions with the healthcare team.
In vitro fertilization (IVF) is a complex fertility treatment that involves ovarian stimulation, egg retrieval, fertilization in a laboratory, embryo development, and embryo transfer. It is a widely used technique to assist couples and individuals in achieving pregnancy. The specific details of an IVF treatment plan can vary depending on individual circumstances, and it is important to consult with a fertility specialist to understand the most suitable approach based on factors such as age, fertility history, and overall health.
Natural, or needle free IVF:
Natural IVF, also known as needle-free IVF or minimal stimulation IVF, is a variation of in vitro fertilization that aims to work with a woman’s natural menstrual cycle without the use of fertility drugs for ovarian stimulation. It offers potential benefits such as reduced cost, lower ovarian stimulation risks, and the option for monthly treatment cycles. However, it is important to consult with a fertility specialist to determine whether natural IVF is the most suitable approach based on individual fertility factors such as a woman’s fertility history, age, and ovarian reserve, and wider goals.
ICSI: Intracytoplasmic Sperm Injection (ICSI):
Intracytoplasmic sperm injection (ICSI) is a specialized technique used in assisted reproductive technology (ART) to address male factor infertility. It involves the injection of a single sperm directly into an egg to facilitate fertilization. ICSI has revolutionized the treatment of severe male factor infertility and has significantly improved fertilization rates and pregnancy outcomes in cases where conventional IVF may not be successful. It is an important tool in ART for couples facing challenges related to male fertility factors.
The process for ICSI is as follows:
- Ovarian Stimulation and Egg Retrieval:
The woman undergoing ICSI treatment undergoes ovarian stimulation using fertility drugs to promote the development of multiple mature eggs. The ovarian stimulation protocol in ICSI is typically similar to that of conventional IVF. Once the eggs have reached an appropriate size and maturity, they are retrieved through a minor surgical procedure known as egg retrieval. - Sperm Collection and Preparation:
On the day of egg retrieval, a semen sample is collected from the male partner or a sperm donor. The sperm sample is then processed in the laboratory to isolate the motile and morphologically normal sperm for injection. In cases where there are severe male factor infertility issues, such as low sperm count or poor sperm motility, additional techniques like testicular sperm extraction (TESE) or sperm aspiration (PESA) may be used to retrieve sperm directly from the testicles or epididymis. - ICSI Procedure:
Under high-magnification microscopy, a single sperm is carefully selected and immobilized using a specialized microscopic needle. The needle is then inserted through the outer shell of the egg (oocyte) and the sperm is injected directly into the cytoplasm of the egg. This precise injection ensures that the sperm bypasses any barriers that may hinder natural fertilization, such as poor sperm motility or abnormalities in the sperm’s ability to penetrate the egg. - Embryo Development and Transfer:
After the ICSI procedure, the fertilized eggs (embryos) are cultured in a laboratory incubator for a period of time to allow for further development. The resulting embryos are monitored for their growth and quality. Typically, after two to six days, one or more embryos of good quality are selected for transfer into the woman’s uterus during an embryo transfer procedure, similar to conventional IVF.
Benefits:
- Male Factor Infertility: ICSI is primarily used to address male factor infertility, such as low sperm count, poor sperm motility, or abnormal sperm morphology. It allows for successful fertilization even when the sperm has difficulty penetrating the egg naturally.
- Increased Fertilization Rates: ICSI has significantly improved the fertilization rates in cases where conventional IVF may have lower success rates due to male factor issues.
- Genetic Concerns: ICSI can be used in conjunction with other specialized techniques, such as preimplantation genetic testing (PGT), to screen embryos for specific genetic conditions before transfer.
Preparation procedures:
Sometimes, preparation work is required before fertility treatments can be carried out. They include:
Hysteroscopy:
Hysteroscopy is a minimally invasive medical procedure that uses a hysteroscope to examine the inside of the uterus. It can be used for diagnostic purposes to investigate various symptoms and identify uterine abnormalities. Additionally, it has therapeutic applications for the removal of fibroids, polyps, and adhesions, as well as the retrieval of displaced IUDs. Hysteroscopy is typically a day surgery procedure performed under local anesthesia, and most women can resume their regular activities shortly after the procedure.
Laparoscopy (keyhole surgery):
Laparoscopy, also known as keyhole surgery or minimally invasive surgery, is a surgical procedure that uses a laparoscope to visualize and operate on structures inside the abdomen, reproductive organs, or pelvis. It is used for both diagnostic and therapeutic purposes and is commonly employed in the treatment of conditions such as endometriosis, fibroids, and ectopic pregnancies. Laparoscopy offers benefits such as smaller incisions, reduced scarring, and faster recovery compared to open surgery. However, it is not without risks, and it’s important to discuss the procedure thoroughly with the surgeon before undergoing laparoscopy.
Diagnostic Uses:
Laparoscopy is commonly used for diagnostic purposes to assess and evaluate various conditions, including:
- Endometriosis: Laparoscopy is considered the gold standard for diagnosing endometriosis, a condition in which the tissue that normally lines the uterus grows outside the uterus. The surgeon can visualize and assess the extent of endometrial implants and adhesions during the procedure.
- Pelvic Inflammatory Disease (PID): Laparoscopy can help diagnose and evaluate the severity of PID, an infection of the female reproductive organs.
- Infertility Evaluation: In cases of unexplained infertility, laparoscopy may be performed to examine the pelvic organs for abnormalities such as blocked fallopian tubes, adhesions, or structural issues.
Therapeutic Uses:
Laparoscopy is also used for therapeutic purposes to treat various conditions, including:
- Endometriosis Treatment: Besides diagnosis, laparoscopy allows for the surgical removal or ablation of endometrial implants, cysts, or adhesions associated with endometriosis.
- Fibroid Removal: Small to medium-sized uterine fibroids can be removed or treated using laparoscopic techniques, such as myomectomy or radiofrequency ablation.
- Ectopic Pregnancy: Laparoscopy can be used to treat ectopic pregnancies (when the fertilized egg implants outside the uterus) by removing the pregnancy from the fallopian tube or other affected areas.